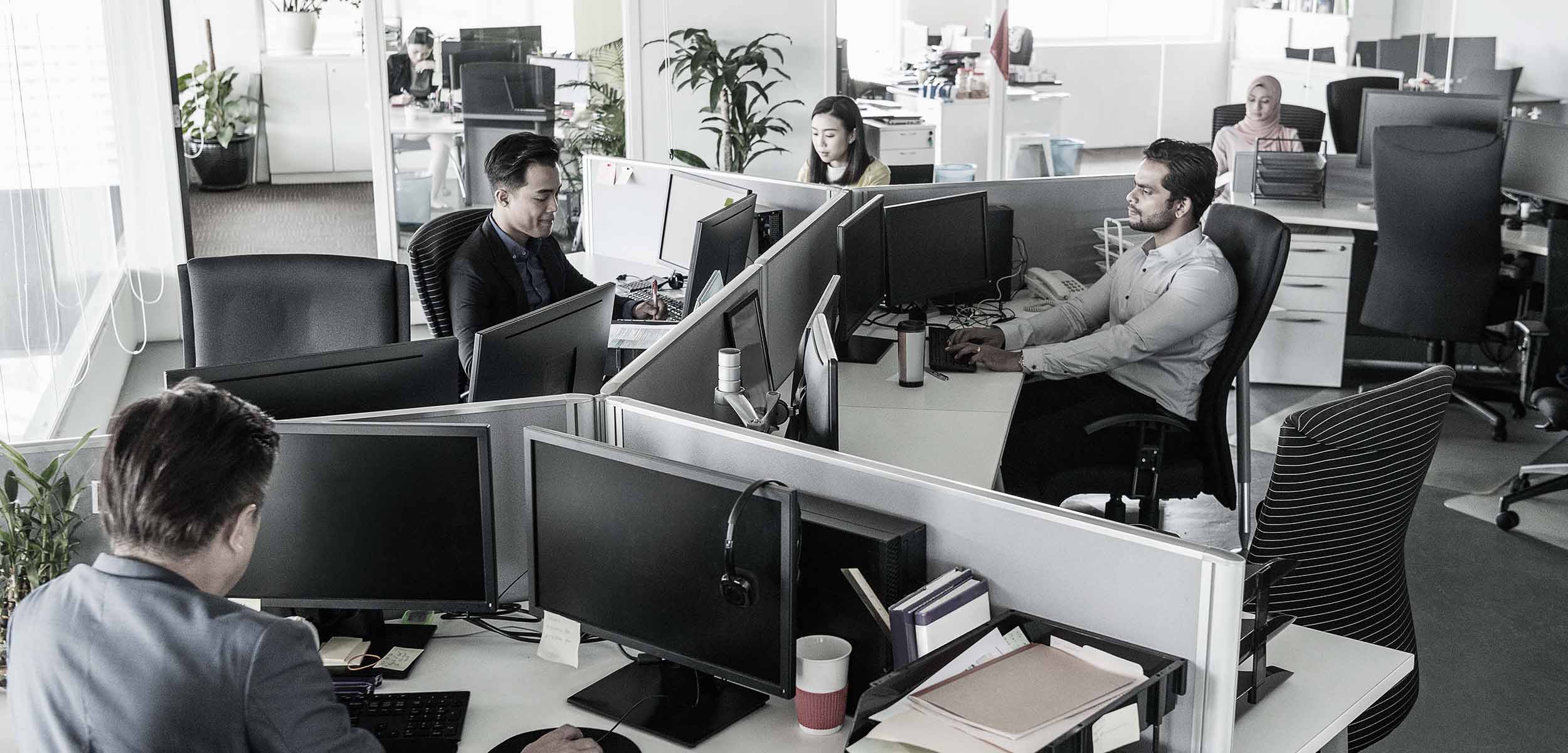
Employer Consolidates Health Plan with Alternatative Funding
Customer Challenge:
A retail distributor with eight branches in three states had been sponsoring three health plans, each separately rated and managed by an HMO. Costs of those plans were expected to increase 24 percent.
Company goals were to:
- offer the same benefits for the same cost to all employees in all locations
- explore self-funding for its health plan
- decrease costs
The client had found that local brokers were not able to effectively consolidate benefit plans across state lines or access necessary data to evaluate self-funding. Large national consulting firms deployed only junior resources, who were inexperienced in managing interstate benefits.
The Liberty Advantage Solution:
Short Term
As a partner, we went into action by first meeting with the client and listening to its goals and objectives to gain a thorough understanding of business needs, company culture, and budgetary constraints. We committed senior experts, who developed short- and long-term plans and were responsible for strategy implementation. As a licensed broker in multiple states, Liberty was able to effectively manage the consolidation.
We analyzed the benefits and costs for each of the three plans to create a consolidated option that took advantage of the client’s collective size. It included a consumer-driven health plan (CDHP) with a health reimbursement arrangement, along with a traditional PPO option that offered employees a choice with costs similar to their previous coverage. Liberty also educated the client on the CDHP, along with self-funding options to consider in the long term.
To help ease the transition, a senior member of our team, who understood both the plan changes and the client’s culture, actively participated in educational meetings at all eight client locations. This full support and service were part of Liberty’s value.
Long Term
After the fully insured consolidation, our team also began analyzing the claims data to assess opportunities for additional savings. After the second year of plan consolidation, the client was faced with a 25% increase from its insurance carrier. Fortunately, we had already been looking at alternative funding methods, educating the client about the advantages of self-funding and illustrating the potential cost impact by structuring the appropriate stop loss levels.
Results
Short Term
First-year participation in the CDHP plan was 50 percent. With the successful plan implementation, the client saved 14 percent in overall costs the first year, and with a favorable loss ratio, experienced a 0 percent rate increase the second year. The total premium savings for the client in year one was 200 percent greater than Liberty’s annual fees, providing an excellent value-to-cost ratio, supported by excellent services and results that exceeded client expectations.
The client’s decision to provide the consolidated plan achieved goals by:
- providing the same benefit options to all employees throughout the multi-state company
- providing premium savings
- offering a health reimbursement arrangement
- added incentives for employees to maintain good health
Long Term
By implementing a self-funded plan for this 400-employee life group, we projected a total plan cost reduction of over $600K for their first year self-funding, with a net savings of $240K over a two-year period. At the end of their first year of self-funding their actual costs were running 23 percent lower than projected, with the additional savings flowing directly to their bottom line. The end of years two and three, they had trend increases to their health plan.
The Power of Negotiation Translates into Cost Savings
Customer Challenge:
An international manufacturer of automotive industry components with employees and retirees throughout eight U.S. states was seeking to:
- Contain its employee benefit costs
- Maintain the richness of its current benefit package
- Retain access to a strong network of physicians and hospitals.
Challenges for this client included the fact that it was without any U.S.-based human resources leadership in the organization. Further, the client was not large enough to receive adequate claim data from the carriers.
The Liberty Advantage Solution:
Because of the client’s staffing situation, our team made the commitment to establish and maintain a proactive, hands-on approach to accommodate the client’s unique needs. We took the time to get to know the manufacturer’s specific challenges, concerns and questions through a focused discovery process to develop a strategic insurance plan and a strong relationship for support.
Year over year, Liberty actively marketed the medical coverage to other carriers on behalf of the client. In doing so, we were able to leverage the competitive quotes for a reduction in the renewal increase.
By gaining a full understanding of its unique needs and advocating for the client when seeking options, the Liberty team was able to present multiple choices, along with recommendations.
Outcome:
Liberty was able to successfully negotiate double-digit renewal increases:
- Year one – from 13.36 percent down to 7.36 percent
- Year two – from 10.5 percent down to 2.32 percent
- Year three – from 9.8% down to 0.00%
The successful negotiations resulted in a $300,000 savings over three consecutive renewal periods. No plan design or carrier changes needed to be made; therefore, the richness of the benefit package was maintained.
High Claims Yielding a High Renewal
Customer Challenge
An international industrial engineering and manufacturing firm headquartered in Belgium with U.S. operations in Ohio and Pennsylvania received a 49.6 percent fully insured renewal increase raising their annual medical costs from $2M to $3M in one year due to large claims.
Their challenge: Offer the same rich benefit levels, keep employee contributions well below benchmarking norms, and increase employer contributions by no more than $200K for each business unit.
The management team was reluctant to move from fully insured to partially self-funded, a funding arrangement they were not familiar with, as well as leave the current network of providers.
The Liberty Solution
Because Liberty was monitoring monthly claim activity, the client was aware and prepared for the large renewal increase. We worked closely with the HR team and other members of the management team throughout the year prior to renewal educating them on consumer driven health plans and self-funding as an alternative funding arrangement.
Liberty evaluated third-party administrators and the networks they offering, and stop loss carriers to protect the client from exposure to catastrophic claims under a self-funded arrangement.
Results
We were able to meet all of the group’s objectives of maintaining the current benefit structure, offering a strong network of physicians and hospitals while maintaining employee contributions well below benchmarking norms.
Liberty senior resources conducted Open Enrollment meetings at each location, providing employees direct access to the lead consultant to ensure a smooth transition of the benefit changes.
The client’s cost under a self-funded arrangement with a third-party administrator and stop loss protection reduced the client’s year one expected costs from the 49.6 percent renewal down to 11.0 percent.